In the last few decades, the world has experienced remarkable advances in healthcare, driven largely by the development of antimicrobial agents such as antibiotics, antivirals, and antifungals. These medications have transformed medicine, enabling the treatment of infections that once claimed millions of lives. However, as these drugs have become more widespread, a new and serious problem has emerged: antimicrobial resistance (AMR). This growing crisis threatens to undermine the significant progress made in healthcare, posing a serious risk to global health, food security, and development.
What Is Antimicrobial Resistance?
Antimicrobial resistance occurs when microorganisms like bacteria, viruses, fungi, and parasites develop the ability to resist the effects of drugs designed to kill them. Over time, these microorganisms mutate or acquire genetic material from other organisms that enable them to survive exposure to antimicrobial agents. The result is that standard treatments become less effective, infections persist, and the risk of spreading resistant microorganisms increases.
For example, antibiotic resistance is a particularly well-known subset of Antimicrobial Resistance. Bacteria like Staphylococcus aureus (responsible for staph infections) or Escherichia coli (commonly associated with urinary tract infections) can develop resistance to commonly prescribed antibiotics such as penicillin, rendering them ineffective. As resistant strains proliferate, treatment options become increasingly limited.
Causes of Antimicrobial Resistance
Several factors have contributed to the rise of antimicrobial resistance, many of which stem from human behaviour and healthcare practices. Some of the primary causes include:
Overuse and Misuse of Antibiotics:
The over-prescription of antibiotics for conditions that do not require them, such as viral infections like the common cold or flu, has accelerated the development of resistance. Similarly, patients often misuse antibiotics by not completing their prescribed course, which allows some bacteria to survive and potentially evolve resistance.
Agricultural Use of Antibiotics:
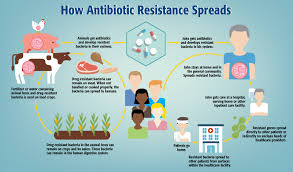
Antibiotics are commonly used in agriculture, particularly in livestock production, not only to treat infections but also to promote growth in healthy animals. This widespread use can lead to the development of resistant bacteria that can be transmitted to humans through the food chain or the environment.
Poor Infection Control in Healthcare Settings:
Hospitals and clinics, where antimicrobial drugs are commonly used, can become breeding grounds for resistant microorganisms. Insufficient hygiene, lack of sanitation, and inadequate infection control practices all contribute to the spread of resistant strains in antimicrobial-resistant healthcare settings.
Lack of New Antimicrobial resistance.
Despite the rising prevalence of resistant infections, the development of new antimicrobial agents has slowed significantly. Pharmaceutical companies have faced challenges in creating new antibiotics, as they are not as profitable as medications for chronic conditions. This has created a dangerous situation where old antibiotics are becoming ineffective, and new ones are not being developed fast enough to replace them.
The Impact of Antimicrobial Resistance
The consequences of antimicrobial resistance are far-reaching, affecting not only individual patients but also healthcare systems and economies worldwide.
Increased Mortality and Morbidity:
AMR leads to higher mortality rates as infections that were once easily treatable become life-threatening. It is estimated that at least 700,000 people die each year due to drug-resistant infections, and this number could rise significantly if no action is taken. Infections that were once routine to treat can now linger, causing prolonged illness and a greater risk of complications.
Longer Hospital Stays and Higher Healthcare Costs:
Drug-resistant infections often require longer treatment, additional tests, and more expensive medications. Hospitals may also need to implement stringent infection control measures, such as isolating patients with resistant infections. This places a strain on already overburdened healthcare systems and increases costs for both patients and healthcare providers.
Impact on Medical Procedures:
Many medical procedures, including surgeries, cancer treatments, and organ transplants, rely on effective antibiotics to prevent or treat infections. Without reliable antimicrobials, these procedures become riskier, with higher chances of complications or even death.
Threat to Global Food Security:
The spread of resistant bacteria in agriculture and food production can affect the safety of the food supply. Crops and livestock are vulnerable to resistant infections, which may reduce food yields and impact the livelihoods of farmers and communities.
Addressing Antimicrobial Resistance
Given the severity of the threat posed by AMR, governments, healthcare providers, the pharmaceutical industry, and the public must work together to address this growing problem. Key strategies to combat AMR include:
Rational Use of Antimicrobials:
Healthcare providers need to prescribe antibiotics and other antimicrobial agents only when necessary and ensure that patients complete their full course of treatment. Public education campaigns can also help raise awareness about the dangers of misuse and overuse.
Infection Prevention and Control:
Improved infection prevention measures in hospitals and other healthcare settings can help reduce the spread of resistant microorganisms. This includes regular handwashing, sterilizing medical equipment, and isolating patients with drug-resistant infections.
Development of New Antimicrobials:
Governments and the private sector need to invest in the research and development of new antibiotics and alternative treatments. This may involve financial incentives for pharmaceutical companies, as well as partnerships with academic institutions and non-profit organizations.
Global Cooperation:
AMR is a global problem that requires a coordinated international response. Countries need to share information on resistant infections, implement standardized surveillance systems, and promote the responsible use of antibiotics in both healthcare and agriculture.
Conclusion
One of the biggest issues facing modern medicine is antibiotic resistance. Without effective action, the world could enter a “post-antibiotic” era where even minor infections become lethal, and medical advances are reversed. By recognizing the severity of the problem and adopting comprehensive strategies to curb the spread of resistant microorganisms, we can protect the effectiveness of antimicrobial agents and safeguard public health for future generations.